Is a mystery of bone.
Joint pain, hair loss and fatigue are data that can point to different conditions. One in particular has thrown people for a loop even when 16,000 new US cases are reported annually.
Lupus is sometimes called a cruel mystery as it may take many years for patients to be accurately diagnosed.
Chronic autoimmune disease is unpredictable and often has delicate symptoms that are easily absent or attributed to other diseases. Meanwhile, uncontrolled inflammation can cause permanent damage.
Here are the symptoms that go through unnoticed and possible treatments at work.
How does lupus happen?
Our immune system protects our body against infections and diseases by identifying and destroying harmful substances. But sometimes our immune system accidentally confuses and attacks our body. We call it autoimmunity – it can lead to inflammation.
The location of the autoimmune attack mainly determines the type of autoimmune disease.
With lupus, you can have inflammation in the joints, under the skin and even in your organs, promoting a wide range of symptoms.

What causes lupus?
We do not know the exact cause of the lupus, but some factors can play a role.
We know that there is a genetic predisposition to the disease and that autoimmune diseases can accumulate in the family, but manifest in different ways. Someone in the family may have psoriasis while another person has thyroid disease and one -third has lupus.
Family history is what we call “first hit”. Often there is a second hit that actually turns into illness and makes it happen to some people. For example, only about 40% of identical twins both have lupus.
It can be something environmental, like exposure to a virus. Sometimes it is exposure to sunlight and UV that activate the immune system and ignite this autoimmune process. We are still trying to discover that mystery.
About 90% of patients with lupus are women, but we are not sure why. Maybe there is a hormonal aspect. We know that patients tend to be lit around their period or after pregnancy, when hormones move.
How is lupus diagnosed?
There is no single test that proves that someone has lupus.
We often start with a blood test of antinuclear antibodies (Ana) that screens for autoimmune disease.
Almost someone with lupus will have a positive result, but a positive result does not confirm a lupus diagnosis.
Rheumatologists also require protein or blood in the urine – which can indicate kidney problems, a common lupus complication – and evaluate the symptoms.
What are the symptoms of lupus?
Patients may have some symptoms of lupus, but not meet the full criteria for diagnosis.
The most common is the pain from the red, hot, inflated joints. There are also some typical lupus rashes.
The butterfly rash passes through the cheek and nose, while the rash of the dispute is dark, circular and scaled. It can occur almost anywhere in the body.
The problem is that joint pains and pain can be tired up to excessive use or muscle damage, and butterfly rash can look very similar to rosacea, which causes redness and redness on the face.
Many of the symptoms are unclear and may not even be part of lupus classification criteria, such as fatigue, hair loss and raynaud syndrome, when fingers or fingers change color in the cold. These symptoms can occur in patients who do not have lupus.
Having lupus should not significantly reduce life expectancy. But while patients live longer, we are becoming more aware that we should pay attention to secondary issues such as heart disease, which may be more common in patients with lupus.
How is lupus treated?
There is no cure for lupus, but it has become an extremely treatable disease by managing the extremely active immune system and reducing inflammation.
A medicine used by almost all our patients is hydroxyklora. It is relatively soft and without many side effects, though we look at issues like long -term eye toxicity.
For many patients, hydroxyl chlorine is not enough. We need to go stronger with immunosuppressive drugs even as the side effects include an increased risk for infections.
We are working on some really promising new therapies. Our research is the exploration of medicines aimed at abnormal parts of the immune system in patients with lupus instead of blanket immunosuppressants that disable the entire immune system. Target therapies mean fewer side effects.
A couple of these medicines have already been approved, and much more are in the pipeline.
Some minor studies suggest that some patients with lupus can reach apologies and get out of medication without experiencing clinical activity. This research is in its infancy, but it gives us hope that one day we can finally say that we have been able to cure this disease.
How can ignition be prevented?
Lupus affects the daily life of almost every patient. They can have a normal day without any symptoms – and things can vary in a currency. The risk of flare may be reduced by:
- Clear direction of sunlight or applying wide spectrum protection with a SPF over 50 because UV rays can activate the disease.
- Confidential stay with vaccinations to reduce the possibility of infections. Anything that lights up in the immune system can also be turned on in the autoimmune process.
- Nutrition of an anti-inflammatory diet. We are learning much more about how our tract GI interacts with our immune system, but it is too early to say which foods to save.
- Avoiding emotional and physical stressors.
Repeated ignitions in the lupus can lead to permanent organs damage and potentially kidney disease.
The good news is that a joint effort by patients, doctors and family members can help maintain symptoms in the breast and hope to put the disease in forgiveness so that patients can live a full and long life.
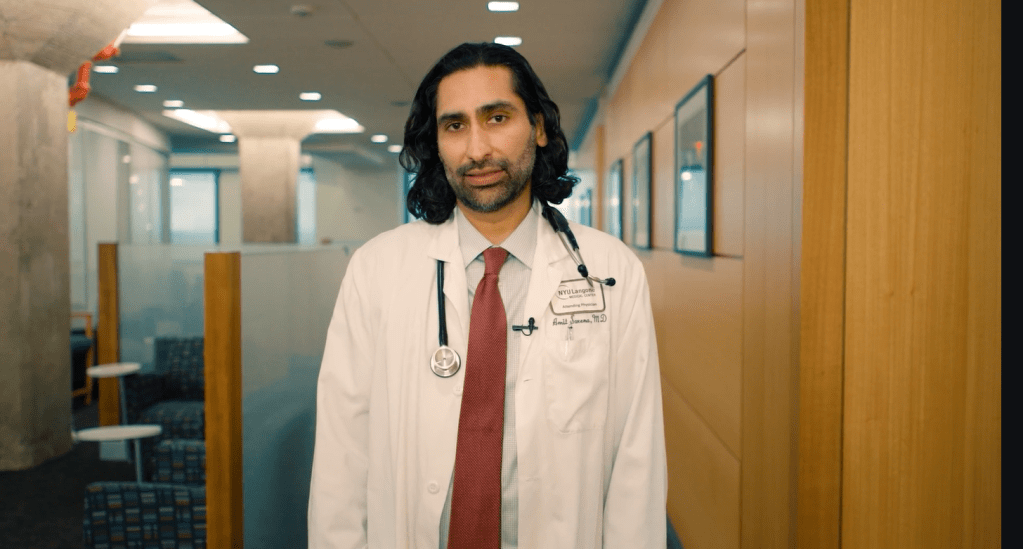
Dr. Amit Saxena is an associate professor in the NYU Langone Health Rheumatology Division. He is also the director of the Rheumatology Clinical Research Program.
#Beware #cruel #disease #mystery #permanently #damage #organs
Image Source : nypost.com